Shoulder Injury Rehab and Prevention for Bowls
Posted on November 10th, 2023 by Andries Lodder
By Marco Mons
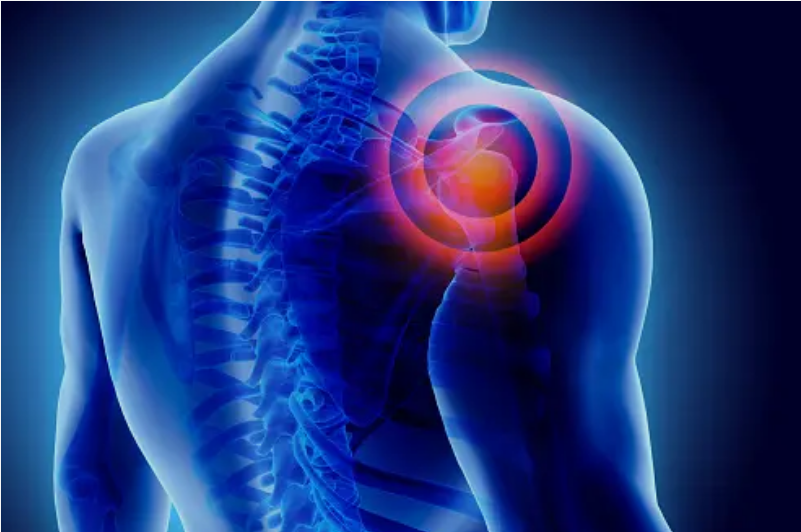
Shoulder injuries in bowls players often result from the repetitive and precise nature of the sport, where accurate throwing and consistent arm movements are crucial. Two of the most prevalent shoulder injuries in this group are rotator cuff injuries and impingement syndrome. Rotator cuff injuries, such as tendinitis or tears, can occur due to overuse and the demands of consistently raising the arm during play. On the other hand, impingement syndrome may develop when the rotator cuff tendons become pinched between the bones in the shoulder, leading to inflammation and pain. Shoulder injury rehab and prevention, through targeted exercise programs, are essential to prevent and manage these injuries among bowls players.
Rehabilitation for shoulder injuries typically involves a combination of exercises, stretches, and lifestyle adjustments. Biokinetics is a field that focuses on improving physical function and quality of life through movement and exercise. To rehabilitate a shoulder injury effectively and prevent future problems, consider the following strategies:
Proper Assessment:
The first step in rehabilitation is to consult with a healthcare professional who can assess the extent and nature of your shoulder injury. A comprehensive evaluation will help determine the specific exercises and treatment plan you need.
Rest and Immobilization:
Some shoulder injuries may require a period of rest and immobilization to allow for healing. This might involve wearing a sling or brace to limit movement while the injury heals.
Exercise:
Under the guidance of a biokineticist, perform a series of exercises designed to strengthen the muscles surrounding the shoulder joint. These exercises help restore mobility, stability, and strength to the injured area. Common exercises may include rotator cuff exercises, scapular stabilization exercises, and range of motion exercises.
Stretching and Flexibility:
Maintaining good shoulder flexibility is essential for preventing future injuries. Stretching exercises help improve range of motion, reduce muscle tension, and increase blood flow to the area. Regular stretching should be a part of your daily routine.
Posture and Ergonomics:
Poor posture and ergonomics can contribute to shoulder problems. Pay attention to your sitting and standing posture and make ergonomic adjustments to your workspace if necessary.
Functional Movement Training:
Biokineticists often use functional movement training to help you regain the ability to perform everyday tasks without pain or discomfort. This involves mimicking daily activities through exercises to ensure a smooth transition back to normal life.
Gradual Return to Activity:
After your shoulder injury has healed, it’s crucial to ease back into your regular activities gradually. Rushing can lead to re-injury, therefore, our biokineticists can provide guidance on the appropriate pace of your return to sports, work, or daily life.
Regular Maintenance:
To prevent future shoulder injuries, continue with a maintenance program that includes regular exercise, stretching, and strength training. Consistency is key to maintaining shoulder health.
Lifestyle Adjustments:
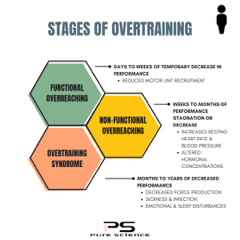
Assess your habits that might contribute to shoulder injuries. Factors such as overuse, repetitive motions, and improper lifting techniques can be modified to reduce the risk of future injuries.
In conclusion, shoulder injuries can be painful and disruptive to your daily life. However, with the correct approach to rehabilitation and a focus on prevention, you can regain strength and mobility while reducing the risk of future injuries. Biokinetics offers a holistic and science-based approach to shoulder health, making it an essential component of your recovery and wellness journey. Consult with a biokineticist to create a customised plan that suits your needs and goals.
Please feel free to contact us on social media or on our website.